Mindfulness is a way of thinking that enhances focus and clarity despite the pressures of a busy day. Mindfulness is especially suited to physicians, because it can help counteract the worrying, perfectionism and self-judgment that are so common among doctors. Meditation training can improve mood and emotion regulation, yet the neural mechanisms of these affective changes have yet to be fully elucidated. We evaluated the impact of long- and short-term mindfulness meditation training on the amygdala response to emotional pictures in a healthy, non-clinical.

Integrating Mindfulness into CBT
By Robert Hindman, Ph.D.
Beck Institute Faculty
A recently published journal article reviewed the empirical support for mindfulness-based interventions for common psychiatric disorders (Hedman-Lagerlof, Hedman-Lagerlof, & Ost, 2018). The authors concluded that the evidence base for using mindfulness-based interventions in the treatment of psychiatric disorders was weak. While other studies have found mindfulness-based interventions to be promising (e.g., Hofmann, Sawyer, Witt, & Oh, 2010), the conclusion of the review article makes sense given how mindfulness is used as part of certain mindfulness-based interventions.
A client of mine I’ll call Tracy had recently completed a mindfulness course, but continued to experience intense symptoms of anxiety. She decided to start treatment with me because she did not benefit as much from the course as she had hoped. Nonetheless, she had enjoyed the mindfulness course, and saw on my profile that I have a background in mindfulness. When I asked her about her treatment goals, the only goal she mentioned was wanting to get rid of the anxiety. This helped me understand why the mindfulness course was not successful. It’s impossible to completely eliminate anxiety because anxiety is a normal part of life.
Mindfulness is a strategy to help people develop a new relationship to experiences such as anxiety, not to eliminate these experiences.
We started treatment by coming up with more realistic and productive treatment goals. Instead of eliminating anxiety, we developed the goal of “learning more helpful strategies for coping with anxiety.” Tracy also had the goal of revising and adapting her mindfulness practice. I asked her, “if anxiety wasn’t a problem anymore, how would your life look different?” Tracy responded that she would accept more invitations from friends to do things that are outside of her “comfort zone,” including hiking, kayaking, and camping. Doing things outside of her comfort zone then became another treatment goal.
I reviewed Tracy’s experience of the mindfulness course, including what she had learned and how she has been applying mindfulness to her life. She reported engaging in mindfulness meditations daily, as well as stopping to meditate whenever strong anxiety arose. While this may seem like a useful strategy, it wasn’t. It actually helped maintain her maladaptive belief: Anxiety causes me to shut down. This occurred because Tracy would stop, leave the situation, and meditate whenever anxiety became intense. The anxiety also lasted longer because her focus was solely on her experience of anxiety instead of whatever was occurring around her. The problem was that the mindfulness training focused on teaching mindfulness to the group without considering Tracy’s individual beliefs. I was able to identify her beliefs as part of her individualized cognitive conceptualization and adjust treatment accordingly.
Instead of teaching Tracy mindfulness meditation with her eyes closed, I taught her how to be more present-focused on the world around her with her eyes open.
My goal for this type of mindfulness practice was to help her be more accepting of the anxiety, while not being excessively focused on it, so that she would be able to continue her activities. The mindfulness meditation first involved her imagining a recent anxiety-provoking situation to elevate her level of anxiety. Next, I placed a paperclip in front of her and guided her through mindfully observing the paperclip while letting the anxiety fluctuate on its own. Through this exercise, Tracy learned how to effectively accept her experience of anxiety, while focusing on the world around her. For her action plan, we decided to have her practice the paperclip exercise daily to further strengthen her mindfulness abilities. She also agreed to use this new version of mindfulness as part of a behavioral experiment. The behavioral experiment tested her belief that anxiety would make her to shut down when hiking on a local trail.
The next session, Tracy reported that her anxiety was high as she got out of her car and was walking towards the beginning of the trail. She then used our version of mindfulness by allowing herself to experience anxiety as she focused visually on the trail and on the scenery. To her surprise, she was able to start the hike, and the further she hiked, the less anxious she felt.

Dialectical Behavioral Therapy Training
Tracy’s experience demonstrates how mindfulness can be more effectively incorporated into therapy when it is individualized according to the client’s cognitive conceptualization.

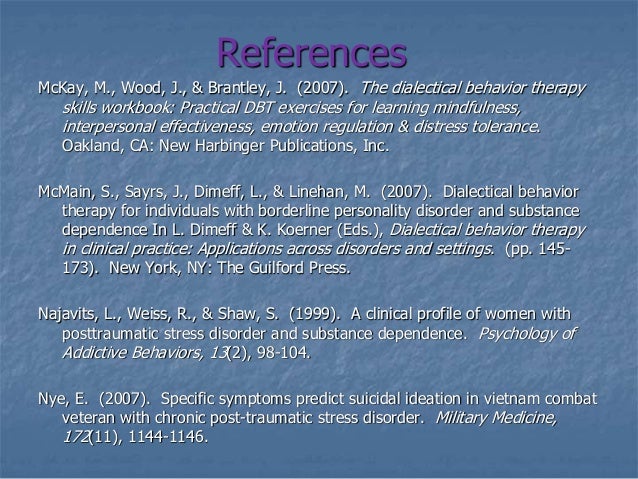
References
Hedman-Lagerlöf, M., Hedman-Lagerlöf, E., & Öst, L. (2018). The empirical support for mindfulness-based interventions for common psychiatric disorders: A systematic review and meta-analysis. Psychological Medicine. https://doi.org/10.1017/S0033291718000259
Hofmann, S.G., Sawyer, A.T., Witt, A.A., & Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78, 169–183.
Upcoming Workshop
03 Mindfulness Overviewdialectical Behavioral Training Center
Integrating CBT and Mindfulness
November 29-30, 2018LEARN MORE

Comments are closed.